CSI is implementing projects on HIV&AIDs prevention and treatment, the main components are voluntary medical male circumcision (VMMC) and ART services at Malual Chaat military hospital in Bor, Jonglei state.
The following are the thematic areas the project is covering;
Demand creation and prevention (VMMC)
CSI will revive prevention services through targeted demand creation: Prevention will remain central to all SSPDF HIV responses. CSI will meaningfully involve military at all levels through community mobilization and monitoring, to encourage uptake and utilization of HIV/health services within Malual Chaat, scaled up to reach at least 90% of those military personnel in need. Current combination HIV programs offered by the SSPDF program include a full range of complementary, acceptable, accessible, quality bio-medical (e.g., condoms, HIV testing, and voluntary medical male circumcision (VMMC)), behavioral, community, social, and structural interventions. The CSI program will be aligned with national, regional, and global guidance developed and supported by the WHO and UNAIDS.
Key activities that CSI is doing under the Demand creation at the facility and in the community.
- At the facility, CSI conduct daily awareness on the importance and availability of vmmc, HST,ART,and VL services
- In the community, CSI conduct daily outreaches to nearby communities and create awareness on the importance and availability of the VMMC, HST, ART, and VL services.
- Daily facilitation and transportation of interested clients to the clinic for circumcision
- At facility, CSI provide water and refreshments to all circumcised clients
- CSI ensures that all the partners eligible PLHIV receive effective screening and tuberculosis preventive treatment (TPT)
- CSI identify clients at risk of HIV infection through screening (age and high risk behaviors, prompting these clients about what they know about PrEP, and routinely
- CSI submit weekly and monthly data report supported with narrative.
ii) Case finding (index testing, targeted community testing and EID)
- Support provision of community based strategies to identify partners and children of HIV positive clients in Bor/ Malual Chaat in line with WHO guidelines and best practices. This targeted community based approach is more cost effective and may reduce the barriers to accessing HIV services by majority of the affected families. All final HIV status confirmation test that yield positive results will be documented and initiated on treatment at MMH or nearby treatment facility.
- The focal person will ensure that identified PLHA (especially mother-baby pairs) are actively linked and retained on treatment at MMH or nearby treatment facility by providing treatment literacy, psycho-social counseling and support services etc. Through anti stigma education sessions, status disclosure, partner involvement and addressing barriers to accessing ART clinic services, the focal person and the CoVs will ensure that all PLHA, including mother-baby pairs have the opportunity to access ART services at the MMH or nearby ART facility.
- Key activities that CSI is doing under case finding
- Mobilize the community to benefit from the HIV/AIDs services at Malual-Chaat.
- To encourage uptake and utilization of HIV/health services within Malual-Chaat.
- To support provision of community based strategies to identify partners and children of HIV positive clients in Bor/Malual-Chaat in line with WHO guidelines and best practices.
- Support the health Officer to follow up lost clients (LTFU) and relink them for treatment at Malual-Chaat military Hospital or nearby treatment facilities. This will be done through; phone call where contacts are available, home visit where addresses are clearly described and at PLHA client monthly meetings.
- To support the health Officer to address the challenges faced by military clients identified to be failing in treatment.
- Documentation and initiation of treatment of all final HIV confirmed test that yield positive result at Malual-Chaat military hospital.
- Ensure that all PLHA, including mother-baby pairs have the opportunity to access ART services at the Malual Chaat Military hospital or nearby ART facility.
- Ensure that identified PLHA (especially mother-baby pairs) are actively linked and retained on treatment at JMH or nearby treatment facility by providing treatment literacy, psycho-social counseling and support services etc.
- Receive updated list of all clients who missed 3 consecutive appointments to track and re-link them for treatment at Malual-Chaat Military hospital or any nearby treatment facility.
- Encourage the identified client to disclose his/her status to their spouse/partners and support those who opt-out of the process; build a support network for PLHA clients including their spouse or other family member/s or trusted friend
- Ensure respect and education of the CSI polices that includes PSEA Policy, safeguarding, Gender, CSI constitution and other policies.
- Continue the community based ARV delivery approach targeting specific clients on treatment at the risk of LTFU due to cost implication.
Work with the community structures and maintain close relationship with the military.
In the community, CSI provide transport support to COVs for community outreach for community testing and escort (mother-infant/HEI) for community DBS samples collection for DNA PCR testing at PHL
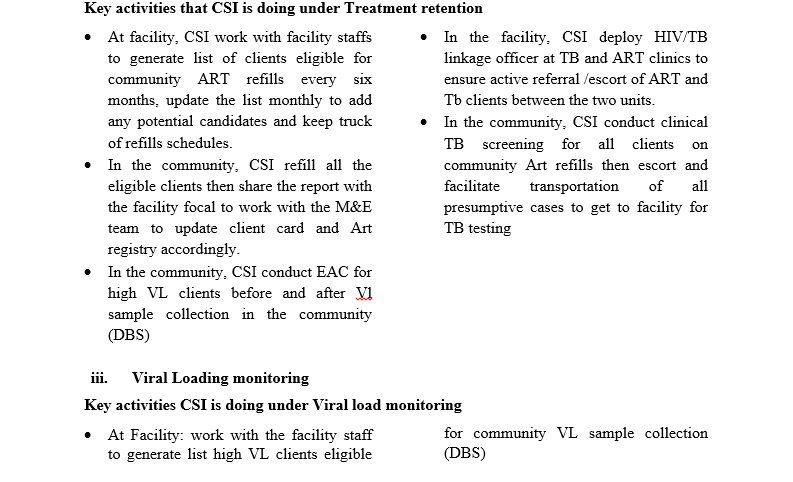
iii). Treatment retention (tracking of IIT, HVL and HIV infected infants plus community ART refill)
CSI work with SSPDF PLHIV groups to support provision of community based strategies to identify partners and children of HIV positive clients in Bor/ Malual Chaat in line with WHO guidelines and best practices. This targeted community based approach is more cost effective and may reduce the barriers to accessing HIV services by majority of the affected families. All final HIV status confirmation test that yield positive results will be documented and initiated on treatment at MMH or nearby treatment facility. The focal person will ensure that identified PLHA (especially mother-baby pairs) are actively linked and retained on treatment at MMH or nearby treatment facility by providing treatment literacy, psycho-social counseling and support services etc. Through anti stigma education sessions, status disclosure, partner involvement and addressing barriers to accessing ART clinic services, the focal person and the CoVs will ensure that all PLHA, including mother-baby pairs have the opportunity to access ART services at the MMH or nearby ART facility